welcome to my sexual health
Credible Sexual Health Providers
Our Website Is Getting a Makeover!
"We're rebuilding to serve you better - thank you for your patience. While we update our online home, we're still here to support you with the same quality sexual health care, world-class resources, and products you trust."
Dr Elna Rudolph, Clinical Head of My Sexual Health

YOUR SEXUAL HEALTH JOURNEY STARTS HERE
Facing Challenges in Sexual Health?
Explore Our Most Trusted Tools for Healing & Pleasure
Need Personal Support or Professional Guidance?
Monthly Live Sessions with Leading Voices
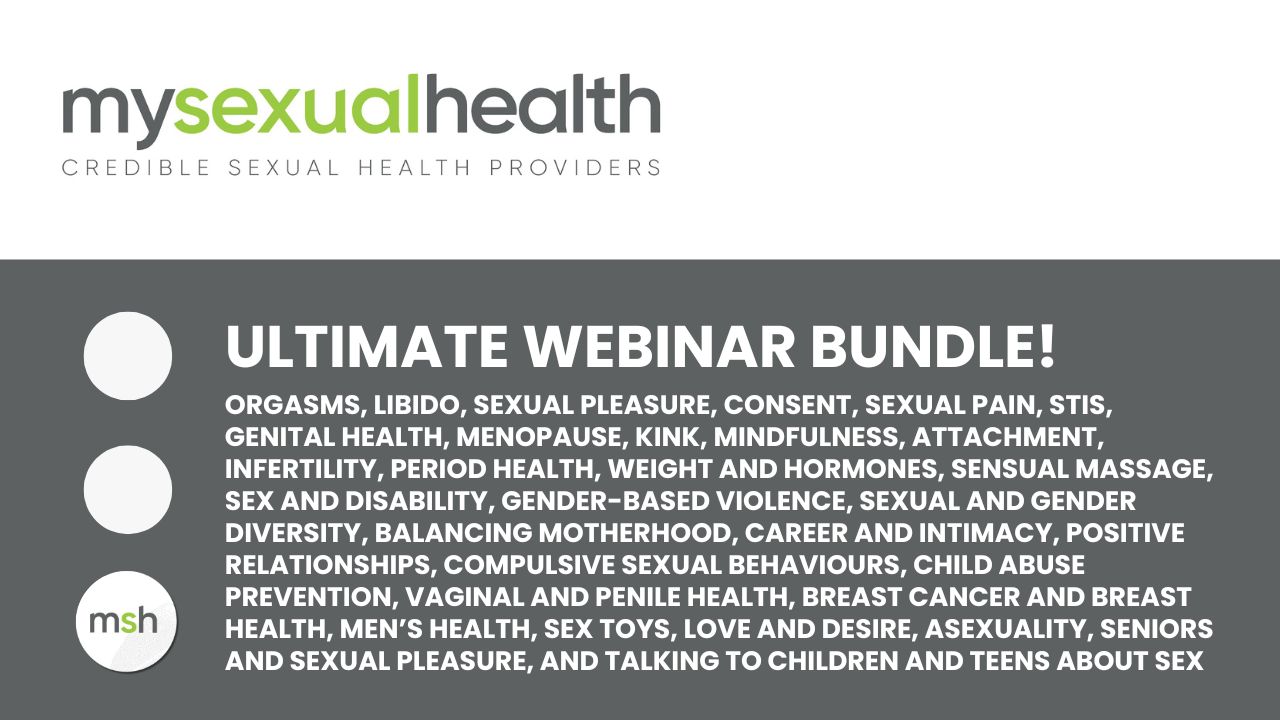
Catch up on all 50+ webinar replays!
The 2025 webinar season has officially wrapped, thank you for joining us this year!
We’ll be back in February 2026 with a brand-new line-up.
In the meantime, you don’t have to miss a thing.
You can access every single replay in our complete bundle, individually valued at R5,700, for just R500.
And here’s the bonus:
When you purchase now, you’ll automatically receive all 2026 webinar replays as they’re released, added straight into this course at no extra cost.
Sign up for our newsletter!
Take the First Step Toward Empowering Sexual Health
Start your journey to better sexual health today
My Sexual Health (MSH)
Credible Sexual Health Providers | Trusted Products | Evidence-Based Education
Based in South Africa, serving patients nationwide
Phone or WhatsApp: +27 (0)61 302 6730
Terms & Conditions | Privacy Policy
© 2025 My Sexual Health | All rights reserved
Find a Practitioner | Shop | Webinars
Sexology Courses | Become Accredited
Join our newsletter for free webinars, sexual health tips, and updates from the MSH Team.
Medical Disclaimer: This site does not replace professional medical advice.
Always consult a qualified healthcare provider.
