welcome to my sexual health
Credible Sexual Health Providers
Our Website Is Getting a Makeover!
We're rebuilding to serve you better — thank you for your patience. While we update our online home, we're still here to support you with the same quality sexual health care, world-class resources, and products you trust. ~ Dr Elna Rudolph
Not sure where to start?
Speak to our Receptionist, Lesli-Anne Smith. She will point you in the right direction. Phone or WhatsApp: +27 (0)61 302 6730

YOUR SEXUAL HEALTH JOURNEY STARTS HERE
Facing Challenges in Sexual Health?
For prescriptions, consultations, or general enquiries:
Email [email protected]
To book mentorship or supervision sessions:
Email [email protected]
Looking for our online courses and webinars?
Visit SexologyCourses.com
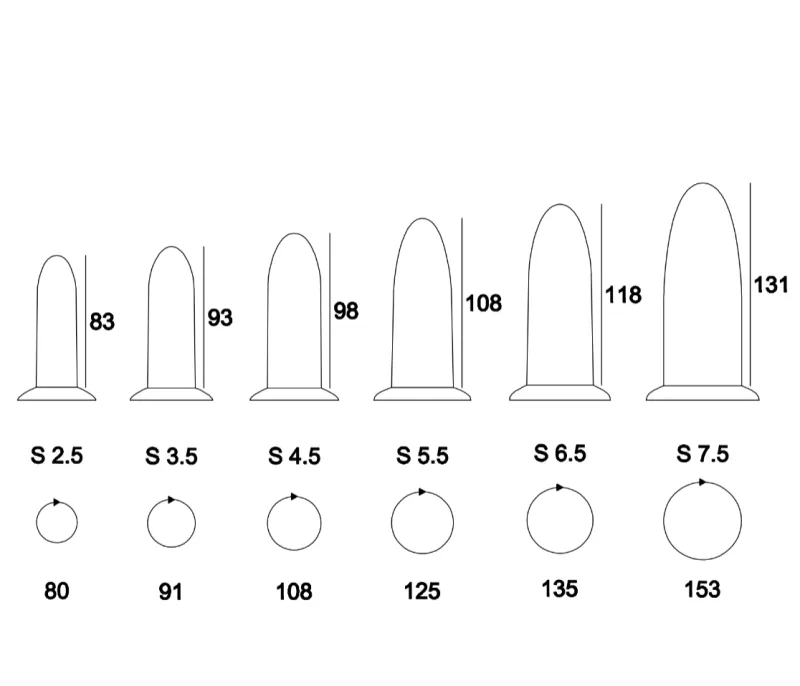
stock up on your favourite products
MSH Shop
Monthly Live Sessions with Leading Voices
Join Our Free June Webinar!
10th June at 8 pm SAST
What Young People Need to Know About Sex & Relationships with Casey Blake – Sponsored by Femagene

Take the First Step Toward Empowering Sexual Health
Start your journey to better sexual health today
Copyrights 2023 | Your Brand™ | Terms & Conditions